Healthy bacteria, healthy skin
As is becoming increasingly clear from recent scientific research, a healthy skin microbiome requires a delicate balance. To take good care of our skin, we need to help beneficial bacteria thrive while at the same time reducing the impact from the microorganisms associated with problems such as acne and eczema.
Contrary to prior beliefs, not all skin bacteria are bad, and common practices once endorsed by practitioners, for example washing your face with strong cleansers to eliminate oil and kill germs, may be doing more harm than good.
The microbiome is now a major focus in the dermatological and cosmetic fields, with researchers working to further understand the mechanisms responsible for healthy skin and its appearance. Scientists now know that many of the microorganisms that thrive on human skin can protect against pathogens and can play an important role in the skin’s innate immune system (1,2). These symbiotic organisms are themselves delicate though and can be wiped out when people use harsh cleansers and certain chemicals, particularly on the face.
Through metabolic processes and in tandem with natural sweat, our beneficial bacterial help to produce the acidic conditions that lead to a healthy skin barrier, known as the acid mantle. Breakdown of the acid mantle, and the concomitant increase in pathogenic bacteria, is associated with skin conditions such as eczema or atopic dermatitis, acne and allergies, among other things (3,4,8) [PM1] [HE2]
The complexity of the facial skin microbiome
The flora and fauna that make up your skin microbiome vary widely depending on the body part and type of skin, and even within different parts of the same body part, for example the face. The varied nature of the skin’s surface — the home of its microbiome — depends on physiological characteristics such as pH, temperature, sebum content and moisture, which are themselves linked to the presence of sweat and sebaceous glands distributed across the skin. It also depends on the so-called topography of the skin, which can be rough or smooth depending on the scaffolding nature of the corneocytes. External environmental factors such as sun exposure, temperature and humidity all play a role as well. All of these factors are reflected in the microbial composition of the skin’s surface, creating a wide range of overlapping variables (5).
Facial skin in particular is a wilderness of diverse microbiota, partly because of this complexity, that has only been partially explored in the literature to date. Facial skin comprises the sebaceous skin types of the forehead, nose and chin — also known as the T-zone — as well as the dry areas of the cheeks.
Because of this lacuna of knowledge around the facial skin microbiome, a team of researchers has conducted clinical studies to assess the bacterial composition of five facial areas and then study what happened to those microbial species when certain bioactive compounds were applied topically to these separate facial areas (7).
Innovation through visualisation
As part of the analysis, the research team recognised the importance of certain visualisation techniques to produce new clarity and insight. They also acknowledged the need to think creatively about the methodology used to examine changes in the numbers of microbes in what could essentially be considered a shifting place and time.
In order to visualise the skin microbiome, various tools have historically been used to measure microbial load and the way it shifts in response to change. One such tool, known as differential abundance or relative abundance, had been considered a gold standard approach despite some controversy regarding its efficacy (6). The methodology requires laborious measurements of total microbial load — practically counting every microorganism — in order to determine shifts in the taxonomy of bacterial colonies. Because of these limitations and because of a desire to gain a deeper, more intuitive understanding of how microbes survive, thrive and interact on the skin, this team of researchers have now turned to a new tool, using a concept borrowed from physics and astronomy, called reference frames.
The concept of reference frames allows researchers to compare relative abundance across samples, and most importantly to observe how those samples shift both in relation to each other and in relation to a common frame of reference, eliminating the need to estimate total microbial load (7). Deploying the concept of reference frames to analyse microbe composition can eliminate false positives and produce consistent results. And perhaps even more interestingly, it can also identify consistent, differentially abundant microbes that often go undetected using conventional analysis.
While current popular methods based on relative abundance can be prone to high false discovery rates, this new methodology constitutes an advancement in techniques that shows promise in handling compositional data and may improve the conclusions we draw (7).
Using the reference frames concept to analyse new generation sequencing data, the research team identified shifts in the microbial composition of study participants’ skin microbiome. They also found that several microbiota were identified as being characteristically associated with the presence of certain bioactive molecules that impact skin health (7).
Cleansing and the skin microbiome
Your skin’s health is also connected to the way it is cleaned, since — as the use of reference frames within the study shows — the ingredients in the cleanser can reduce certain populations of bacteria while increasing others. The team investigated the effect of skin cleansing with a body wash containing saccharide isomerate, also known as Pentavitin®, which is a well-known cosmetic ingredient that contains a unique binding mechanism to the skin that is used for both short and long-term moisturisation. This hygroscopic compound retains water but can also be metabolised by the local microbiota.
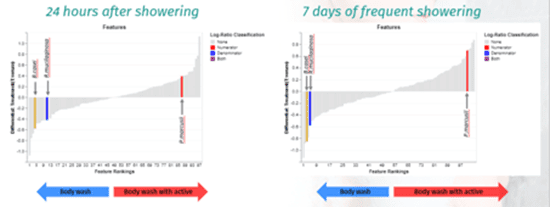
Researchers used reference frames to identify specific, differentially abundant microbial families that stayed on the skin, at all the timepoints evaluated, when volunteers used a body wash that contained saccharide isomerate (7).
When you cleanse your skin you are mechanically and chemically removing dirt and pollutants, as well as microbiota. And while skin cleansing can help maintain good skin health, protect us from infections, illness and ailments, cleaning can also strip away oils and moisture. This potentially leads to irritated skin, a breakdown skin’s function as a natural barrier and a disturbance in the skin’s microbial composition.
In order to examine skin cleansing’s impact on the microbiome, this team of researchers enrolled 30 Caucasian women in a placebo-controlled clinical study, where they applied a liquid body wash twice daily for one week to the underside of their forearms in order to mimic frequent showering. The study revealed changes to the microbiome due to cleaning and allowed researchers to assess the beneficial effects of saccharide isomerate on participants’ skin.
Even though the cleansing process created both a short-term and long-term change in the microbiome composition, the skin microbiota proved resilient, and were able to re-establish themselves and adapt to the new environment. Interestingly, the use of saccharide isomerate in the body wash was associated with the reduction of so called “coryneform” bacteria such as B.casei and R.mucilaginosa, which are increasingly implicated in skin infections (7). It also showed the enrichment of a beneficial but often overlooked bacterium, P.marcusii. P. Marcusii is a particularly interesting organism with abilities to degrade, detoxify and disable contaminants.
Sebum and the skin microbiome
Alongside the facial cleansing study, researchers also looked at the effect on oily skin of a cosmetic regimen derived from a plant extract, Epilobium fleischeri, that is known for its sebum-regulating properties.
Sebum, the oily, waxy substance secreted by skin’s sebaceous glands, is a mixture of fatty acids, sugars, waxes and other chemicals that together help to retain moisture in the skin and protect against evaporation. Similar to the impact of over-cleansing or cleansing with suboptimal ingredients, an imbalance in your skin’s sebum production can also lead to acne and dermatitis.
Sebum production varies by skin type and body part— the face alone has different regions where sebum production can be higher or lower, with levels particularly strong in the the T-zone.
To examine the ways in which the skin microbiome and sebum production interact, the researchers conducted a clinical study that looked at the bacterial composition of five different facial areas and the ways in which the plant extract Epilobium fleischeri impacted the microbiota on facial skin. The team focused on overall skin improvement after applying a formulation of Epilobium fleischeri known as Alpaflor® Alp-Sebum, and they looked at how the improvements were reflected in the make up of the skin microbiota on different parts of the face.
They enrolled participants with oily skin and excess sebum production, as they were curious to discover whether and to what extent the plant extract helped people with acne-prone skin. The study also allowed them to assess how much the plant extract could help, and it also allowed them to map microbial changes in response to product application.
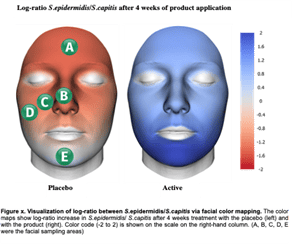
Based on the study, researchers were able to conclude that participants’ overall skin condition was improved by modulating key bacteria on all facial sites that had a balanced facial microbiome. Enlarged pores, skin inflammation irritation and redness were all reduced when the levels of S. capitis, C. kroppenstedtii, C. avidum and C. tuberculostearicum were reduced.
Conversely, facilitating the maintenance and growth of S. epidermidis, S. hominis and M. yunnanensis promoted microbial skin self-defence by protecting against growth and colonisation of pathogenic bacteria. They found that C. acnes was not particularly modulated by Alpaflor® Alp-Sebum. The majority of C. acnes strains are non-pathogenic and an essential part of the facial microbiome as they help to block pathogens. Only a few strains are in fact pathogenic and associated with acne.
The delicate balance
When dealing with the challenges of acne and other troublesome, persistent skin issues such as eczema, seborrheic dermatitis, dry, red and irritated skin and dandruff, it is of paramount importance to keep in mind the delicate balance our skin microbiome needs in order to thrive.
People using conventional skin cleansing and care regimes, as well as other beauty products and cosmetics, can unwittingly accelerate the very damage they are trying to prevent when they ignore the impact of those products on the skin microbiome. Evidence is increasingly pointing to the connection between microbiota misbalances, or dysbiosis, and certain conventional skin care products.
Product suppliers and manufacturers should help consumers care for their skin, and their naturally beneficial bacteria, by focusing on developing ingredients that maintain balance and microbial harmony.
Certain microbiome friendly certified ingredients are now available, including 1,3-propanediol, niacinamide, several hyaluronic acid grades, Epilobium Fleisheri and saccharide isomerate, among others.
The growth in scientific research around the skin microbiome has also fostered the development of certified finished formulations such as shampoo, serums, day creams as market-ready solutions for consumers.
These products have been shown to provide a microbiome-friendly solution to common skin conditions. They can help our skin — and our skin’s microbiome — do the job it was designed to do and maintain that healthy balance.
References
- Sanford JA, Gallo RL. Functions of the skin microbiota in health and disease. Seminars in immunology. 2013;25(5):370-7.
- Belkaid Y, Segre JA. Dialogue between skin microbiota and immunity. Science (New York, NY). 2014;346(6212):954-9.
- Lambers H, Piessens S, Bloem A, Pronk H, Finkel P. Natural skin surface pH is on average below 5, which is beneficial for its resident flora. International journal of cosmetic science. 2006;28(5):359-70
- Elias PM. Stratum corneum acidification: how and why? Experimental dermatology. 2015;24(3):179-80
- Findley K, Oh J, Yang J, Conlan S, Deming C, Meyer JA, et al. Topographic diversity of fungal and bacterial communities in human skin. Nature. 2013;498(7454):367-70.
- Morton, J.T., et al., Establishing microbial composition measurement standards with reference frames. Nat Commun, 2019. 10(1): p. 2719
- Sfriso R, Clypool J. Microbial Reference Frames Reveal Distinct Shifts in the Skin Microbiota after Cleansing. Microorganisms. 2020
- Luebberding, S., Krueger, N. & Kerscher, M. Age-related changes in skin barrier function—Quantitative evaluation of 150 female subjects. Int. J. Cosmet. Sci. 35, 183–190 (2013).
