Let’s start with a question, what is healthy skin?
The definition is broad, but it generally consists of three elements: touch, look and perception. Common associations that we come across include smooth skin that is not too sensitive, dry or flaky, or too oily. Most of us seek a healthy glow, and to prevent and treat skin conditions such as eczema and rosacea.
In line with this, the beauty and personal care market offers a range of products that aim to protect and rejuvenate your skin so you can achieve and maintain a healthy condition, using a diverse array of methods such as cleansing, exfoliating and moisturizing. What these products all have in common is the fact that they all act on your body’s outermost layer – the skin barrier.
But what exactly is your skin barrier, and how does it contribute to the condition of our skin?
Here we will take you through our skin health 101 – exploring the skin barrier and various processes that contribute to the health and condition of our skin, with particular focus on dry, oily and sensitive skin, as well as the influence of the skin microbiome.
The structure and protective power of our skin
Your skin is made up of layers, each of which performs important functions in protecting your body (read this to get the full picture on skin structure).
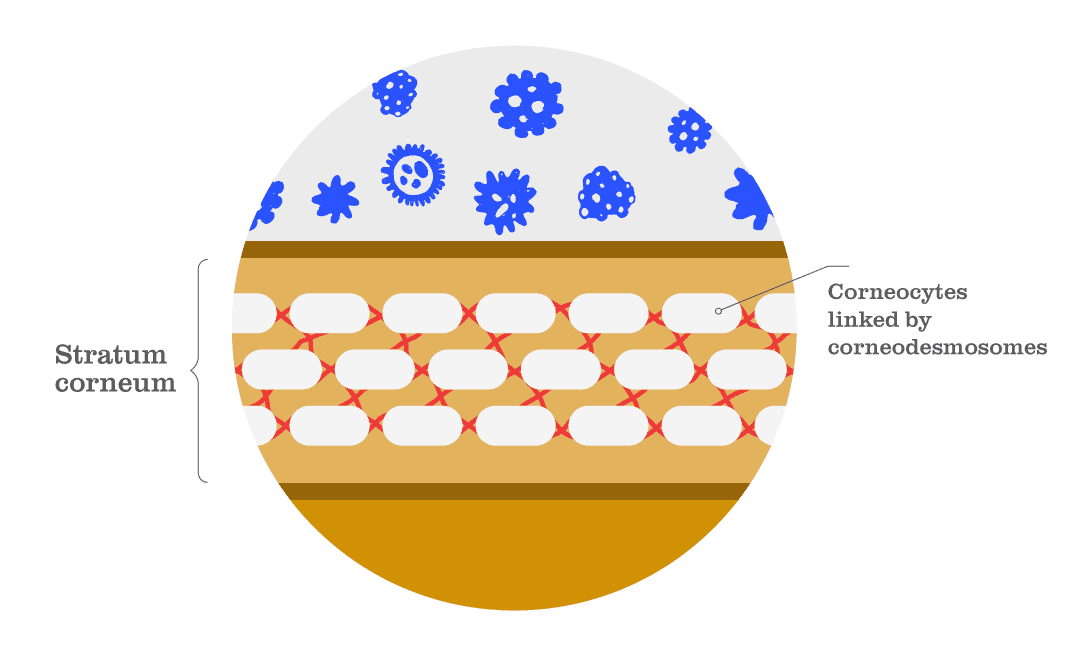
The outermost layer of the skin, the epidermis, acts as a protective barrier. It serves multiple functions, which are largely attributed to its top layer of cells: the stratum corneum. The stratum corneum consists of ‘corneocytes’ (a type of skin cell) supported by ‘corneodesmosomes’ (a type of skin protein) and other crosslinked proteins and lipids. These components form a wall that acts as a highly effective barrier to protect against the external environment and threats such as dehydration and pollution (Fig. 1).
This outer skin barrier is essential for good health and needs to be protected to function properly. Without it, harmful allergens, toxins, irritants and pollutants from the outside environment, as well as threatening pathogens, could penetrate your skin and wreak havoc in your body. It also protects us from exposure to harsh chemicals in products, and provides a shield against humid and dry environments, preventing the water inside your body from escaping and evaporating, and against harmful UV rays of the sun. However, on the flipside, the skin barrier can itself suffer from these threats, and due to hygiene issues such as over-washing and over-exfoliating.
When your skin barrier isn’t functioning properly, you may be more prone to developing the following skin conditions [1]:
- Dry, scaly skin
- Itchiness
- Rough or discoloured skin
- Sensitive or inflamed skin
- Bacterial, viral or fungal skin infections
The skin microbiome also plays a role here, with imbalances in composition (dysbiosis) associated with several skin disorders, such as eczema, acne, allergies and dandruff, as well as sensitive, irritated, inflamed and dry skin [2].
To get a better understanding of how skin barrier function contributes to skin health, and subsequently the role of the skin microbiome, let’s explore some examples in more detail…
Dry skin
Dry skin – also known as xerosis – is a common ailment, especially in older adults.
Dry skin has been linked to low temperature and humidity, as well as high exposure to UV radiation from the sun (find out more about UV here), all of which have been shown to impair the skin barrier [3]. Facial and hand skin also seem to be particularly affected – why is this, and what exactly is going on in the skin barrier?
Well, dry skin can emerge under a range of conditions that affect the ability of the epidermis to store and hold water. When lacking water, the stratum corneum becomes more rigid, influencing the physical properties of the skin and impacting skin barrier function [4]. One reason that the face and hands are particularly prone to dry skin, is that the skin barrier of the areas is markedly different from other areas of the body. Cheek skin, for example, has smaller corneocytes (those skin cells shown in Fig. 1), thinner cell layers and reduced levels of natural moisturizing factors (which are essential for hydration of the stratum corneum and a stable skin barrier) relative to the skin of other body sites [5,6]. These differences in skin composition make areas such as the cheek and skin more susceptible to dryness.
As well as natural variations in skin composition, proteins such as ‘fillagrin’ can contribute to dry skin. When this protein is present at normal levels, we can expect a healthy, functioning skin barrier. Fillagrin condenses the keratin skeleton within skin and contributes to the formation of squames – flakes of skin. Within the squames, fillagrin also breaks down into amino acids that are key for the production of natural moisturizing factors, which help keep the outer layer of the skin protected and well-hydrated [7]. However, loss or disruption of filaggrin production (for example, due to genetic mutations in our cells) leads to a poorly formed stratum corneum that is also prone to water loss, and there is even increased risk of atopic dermatitis (the most common form of eczema) [4,7,8]. The protein is also key for the defensive nature of the skin barrier as it helps protect the body against entry of allergens and other foreign substances [7].
Dry skin is also thought to worsen depending on season, and is particularly bad in winter – it has been found that during the winter in northern countries, the risk of dermatitis (itchy, dry skin) is increased due to low temperature and humidity, and it is particularly common on weather-exposed skin such as the cheeks and hands [4]. Variations have also been found in association with age and gender [4], and research has shown that factors such as skin hydration and pH can vary greatly even across small distances of the face, and that these gradients are distinctive amongst different ethnic groups [9].
With numerous underlying biophysical processes, and an array of contributing factors such as skin type, age and gender, more work is needed to understand the full mechanics of dry skin. It remains a major concern globally despite decades of moisturizer development, but it is now clear that skin moisturization is more complex than simple skin hydration. New types of treatments, based on ingredients such as lipids, niacinamide and humectants, may be the key [4].
Oily skin
Oily skin – another common dermatologic concern – is a result of excessive sebum production [10].
Sebum is an oily, waxy substance produced by your body’s sebaceous glands. It coats, moisturizes and protects your skin, and is the main ingredient in your body’s natural oils. Sebaceous glands are usually connected to hair follicles, and are highly concentrated behind the ear and on the face, upper chest and back (which happens to be the same distribution as acne…).
The amount of sebum a person produces varies throughout the course of their life. Following relatively high production at birth, sebum levels then decrease until puberty, at which time production dramatically increases. Sebum production does not decline again until after menopause for women, and around the sixth to seventh decade for men. The average rate of sebum production in adults is 1 mg per 10 cm2 of skin every three hours. When rates fall below 0. 5 mg, this is another factor that can contribute to dry skin. However, when sebum production exceeds 1.5 mg, the excess results in oily skin [10].
Several factors have proposed to help explain why the skin of some individuals might appear more oily than others. Men in general have higher sebum output, attributed to higher testosterone levels, although sebum production does increase during ovulation in women [11]. Sebum also varies according to the external environment and the time of year, with several research studies describing an increase in sebum production during the spring and summer and in more humid climates [12,13]. Race and ethnicity can also have an impact – Chinese women display notably smaller pore size, while Black individuals general have a larger pore size that can be attributed to higher sebum production [14,15].
Sensitive skin
Sensitive skin is generally used to describe skin types that are experience abnormal sensory perceptions, such as stinging, burning, tingling, pain and itching, and skin that has low tolerance to beauty and personal care products.
Sensitive skin conditions can vary by type and symptoms, but can occur in individuals with normal skin or as a part of the symptoms associated with skin disorders such as rosacea, atopic dermatitis and psoriasis (particularly on facial skin).
The mechanics of sensitive skin are poorly understood, but there are a few different underlying processes that are thought to contribute to the various types of sensitive skin [16,17] – two key examples are:
- Skin barrier disruption. Disrupted skin barrier function is thought to lead to skin sensitivity as altered lipid concentrations and disruptions across other skin barrier components can cause skin discomfort. Increases in ‘sphingolipids’, for example, have been linked to reduced barrier stability. A weak skin barrier facilitates the penetration of irritants or allergens, and increases transepidermal water loss (TEWL) – of which can lead to skin discomfort [17].
- Skin nervous system disruption. Due to the wide variety of sensory symptoms associated with sensitive skin conditions, such as burning, tingling, stinging, pain and itching, it is likely that nervous system dysfunction in the skin might be one of the mechanisms at work when it comes to skin sensitivity. For example, sensitive skin sensations might result from an insufficient protection of nerve endings due to an impaired skin barrier, or from an increased density of nerve fibres in the skin. Atopic dermatitis, for instance, can cause itching and tingling, and has been shown in association with higher skin nerve densities relative to individuals with healthy skin [17].
Our skin is subject to numerous factors that are thought to contribute to sensitive skin conditions. This includes physical factors (such as UV radiation, heat, cold and wind), chemical factors (cosmetics, soap, water and pollution), lifestyle factors (diet and alcohol consumption), psychological factors (stress) and hormonal factors (menstrual cycle) [16,17,18].
UV radiation, for example, was identified as potential contributing factor as sensitive skin prevalence increases during summer, when we undergo increased UV exposure. In support of this theory, fair-skinned individuals prone to sunburn have reported increased discomfort compared to those with darker skin [17].
So, sensitive skin conditions are diverse in how they manifest and the underlying causes. Although often transient, and occurring without any visual ailment, prevalence is high. Approximately 39% of the population in Europe are affected, and sensitive skin conditions can have a significant impact on quality of life, so management should be a top priority within beauty and personal care [17,18].
The role of the skin microbiome
When looking at the role of the skin microbiome in skin health, it is first important to understand that this is a two-way dynamic relationship – healthy skin is essential to support a healthy microbiome, and having a balanced skin microbiome also contributes to skin barrier function and helps to support and maintain a healthy and stable skin environment [19].
Allow us to explain…
Healthy skin for a healthy skin microbiome
Healthy human skin is colonized with a diverse population of microorganisms [20].
Across the body, the skin can be naturally divided into moist, dry and sebaceous (oily) sites, and each of these skin site types has its own distinct microorganism ecosystem. There are similarities in terms of bacterial species – for example, all sites share Cutibacterium, Corynebacterium and Staphylococcus bacteria – but with some variation in stability, abundance and distribution patterns [21,22].
Sebaceous and moist skin sites exhibit a very stable composition over time. Dry skin sites are more unstable partly due to the low number of bacteria present, limited nutrients available, and increased sensitivity to environmental conditions [21,22]. This also means that when normally moist environments grow drier, issues can arise. Hydrated skin, for example, allows a healthy microbiome to thrive. Dry skin can lead to overgrowth, survival and invasion of problematic bacteria to the detriment of other resident skin bacteria, which can result in inflammation and reduce the benefit of a healthy microbiome.
Skin barrier integrity and function play a key role here, as they have been shown to affect the skin microbiome composition. Skin lipid composition, for example, is strongly correlated with microbiome composition, and skin with decreased filaggrin levels (which we know is typical of dry skin) shows a distinct microbiome composition that has also been linked to atopic dermatitis [23].
A healthy skin microbiome for a healthy skin barrier
On the flipside, the skin microbiome itself can be viewed as a core component of skin health, as it can influence skin barrier function and our immune responses [24].
Skin-resident microbes, for example, help maintain a stable skin environment and can regulate our inflammatory response or trigger an immune reaction when threatened [25]. However, if disrupted, variations in our normal skin microbiome composition can lead to inflammation, irritation, dryness, itchy skin and worsen our skin condition, challenging our immune systems. This may also contribute to the progression of inflammatory skin conditions such as acne, atopic dermatitis and psoriasis as a result of an unregulated inflammatory response (read more about the skin microbiome and immunity here). For example, one part of our immune response known as the ‘Toll-like receptor pathway’ can be overstimulated by the presence of certain microorganisms when they trigger activation of the pathway as a defensive immune response, leading to inflammation [26].
The skin microbiota also plays a major role in the function of the skin as a barrier against environmental stressors [24,25]. For example, the skin microbiome has been shown to help mediate the adverse effects of air pollution on skin health [24], and to play a protective role when it comes to harmful UV rays – skin resident bacteria (along with fungi) can produce UV-absorbing biomolecules as protection, while also providing antioxidant and anti-inflammatory properties (find out more here).
This mutualistic relationship between microbial communities and us as hosts is therefore essential to establish the well-controlled and delicate balance needed for healthy skin, and so the role of the skin microbiome in mediating skin physiology remains a growing area of research in science [24,25].
Explore more microbiome basics in the How it works section of the Content Hub and follow us on Instagram for the latest updates!
References
- https://www.healthline.com/health/skin-disorders
- Sfriso, R. et al. Revealing the secret life of skin – with the microbiome you never walk alone. Int. J. Cosmet. Sci. 42, 116-126 (2019).
- Engebretsen, K. A. et al. Changes in filaggrin degradation products and corneocyte surface texture by season. BJD https://doi.org/10.1111/bjd.16150(2018).
- Voegeli, R. & Rowlings, A. V. Moisturizing at a molecular level – the basis of corneocare. IFSCC 24, 4 (2021).
- Egawa M, Tagami H. Comparison of the depth profiles of water and water-binding substances in the stratum corneum determined in vivo by Raman spectroscopy between the cheek and volar forearm skin: effects of age, seasonal changes and artificial forced hydration. Br J Dermatol 158:251–60 (2008).
- Machado M, Hadgraft J, Lane ME. Assessment of the variation of skin barrier function with anatomic site, age, gender and ethnicity. Int J Cosmet Sci 2010; 32:397–409.
- Sandilands, A. et al. Filaggrin in the frontline: role in skin barrier function and disease. J. Cell Sci. 122, 1285–1294 (2009).
- Irvine AD, McLean WH, Leung DY. Filaggrin mutations associated with skin and allergic diseases. N Engl J Med 365:1315–27 (2011).
- Voegeli, R. et al. Facial skin mapping: from single point bio-instrumental evaluation to continuous visualization of skin hydration, barrier function, skin surface pH, and sebum in different ethnic skin types. Int. J. Cosmet. Sci. 41, 411-424 (2019).
- Endly, D. C. & Miller, R. A. Oily skin: a review of treatment options. J. Clin. Aesther. Dermatol. 10, 49-55 (2017).
- Wm, B. Y. et al. Sebum, acne, skin elasticity, and gender difference- which is the major influencing factor for facial pores? SkinRes Technol. 19, E45–53 (2013).
- Man, M. Q. et al. Variations of skin surface pH, sebum content,and stratumcorneum hydration with age and gender in a large Chinese population. Skin Pharmacol. Physiol. 22, 190–199 (2009).
- Wan, M. J. et al. Seasonal variability in the biophysical properties of forehead skin in women in Guangzhou City, China. Int. J .Dermatol. 54, 1319–1324 (2015).
- Roh, M. et al. sebum output as a factor contributing to the size of facial pores. Br. J. Dermatol. 155, 890–894 (2006).
- Sugiyama-Nakagiri, Y. et al. Ethnic differences in the structural properties of facial skin. J. Dermatol. Sci. 53, 135–139 (2009).
- Miser, L. et al. Sensitive skin: psychological effects and seasonal changes. J. Eur. Acad. Dermatol. Ven. 21, 620-628 (2007).
- Misery, L., Loser, K. & Stander, S. Sensitive skin. J. Eur. Acad. Dermatol. Ven. 30, 2-8 (2016).
- Jiang, W. et al. Seasonal changes in the physiological features of healthy and sensitive skin. JCD 10.1111/jocd.14476 (2021).
- Boxberger et al. Challenges in exploring and manipulating the human skin microbiome. Microbiome. 9, 125 (2021).
- Futter, T. et al. Assessment of skin microbiome diversity and skin health in dry skin and dry, itchy skin: A bilateral, controlled clinical trial using oat-containing lotions and wash. AAD https://doi.org/10.1016/j.jaad.2019.06.121 (2019).
- Callewart, C. et al. Skin microbiome transplantation: current state of the art. Comput. Struct. Biotech. J. 19, 624-631 (2021).
- Byrd, A. L. et al. The human skin microbiome. Nat. Rev. Microbiol. 16, 143-155 (2018).
- Baurecht, H. et al. Epidermal lipid composition, barrier integrity, and eczematous inflammation are associated with skin microbiome configuration. J. Aller. Clin. Immunol. 141, 1668-1676 (2018).
- Wang, L. et al. Facial Skin Microbiota-Mediated Host Response to Pollution Stress Revealed by Microbiome Networks of Individual. mSystems 6, e00319-21 (2021).
- Luna, P. C. Skin microbiome as years go by. Am. J. Clin. Dermatol. 21, 12-17 (2020).
- Kumar, V. Going, Toll-like receptors in skin inflammation and inflammatory diseases. EXCLI J. 20, 52–79 (2021).
