Towards the end of 2021, we decided to explore the topic of aging.
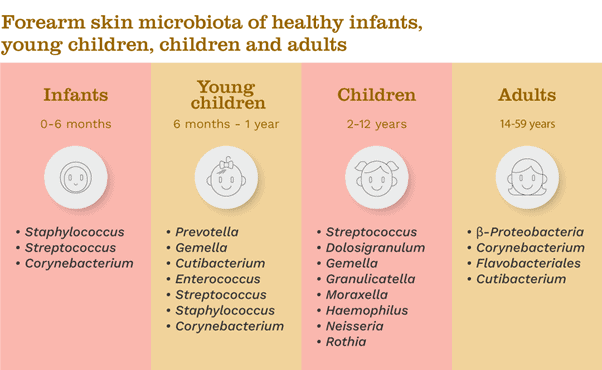
As our contributor Dr Lionel Breton explained, the skin microbiome of individuals changes and increases in diversity as we grow from early age to adulthood, with the variations also linked to skin health and condition. Here we provide a brief recap, and hunker down on one period in detail – the postnatal microbiome.
The microbiome during the postnatal period and through infancy is distinctly different to that of adults, and it follows that the contributions of microbes to skin health and disease during our early years of life may be unique as well. It is therefore critical to understand the postnatal skin microbiome and how it evolves across the early years of our life to understand the best way to care for infant skin…
The aging skin microbiome
Research investigating the skin microbiome of individuals ranging from young to old age has shown a change in skin microbiome composition from infancy to adolescence [1], as well as differences according to the living environment [2,3].
Skin bacteria samples of younger (<35 years) and older (>60 years) women in Japan, for example, have revealed that skin microbiome composition and diversity are strongly affected by age. A higher diversity was observed in older skin relative to younger skin, and the samples from the forearm were particularly diverse [4].
Although the reasons are likely to be multi-factorial, these differences could arise because less nutrients are typically available on older skin, due to age-associated reductions in skin cell renewal, sweat and sebum secretion and a weakened immune function, which can lead to the demise of the dominant bacteria and increases in other ‘opportunistic’ species [4,5,6,7].
For a full recap on microbiome changes from infancy to adolescence, see our blog here. However, if we go back to the very start of infancy, to the postnatal microbiome – what is going on here?
The postnatal skin microbiome
The dynamic nature of the skin microbial communities (the microbiota) is apparent from the very early stages of life, following initial exposure to the maternal microbiome [8]. Birth itself marks a time of drastic change for the skin, as the newborn undergoes a sudden transition from an almost bacteria-free aqueous environment to an atmospheric one, with constant exposure to microbes.
The environmental conditions encountered at and immediately after birth therefore significantly influence the development of the postnatal microbiome, with the initial colonization of a newborn baby’s skin first depending on the mode of delivery. Children born naturally acquire larger abundances of vaginal bacteria (Lactobacillus and Candida albicans), while those born by caesarean section acquire skin microbes (Staphylococcus and Streptococcus) [9,10,11].
Within a few hours of birth, neonatal skin structure plays a key role in skin microbiome development. Immaturity in skin structure and function, for example, dependent on gestational age, can result in impaired skin barrier function and thus disrupt skin microbiome development [12,13]. The stratum corneum (the outermost layer of skin) is a crucial part of this as it is responsible for both structural and immune protection. In premature infants, an immature stratum corneum means increased skin permeability, temperature fluctuations, water loss, electrolyte imbalances and risk of infection [12]. This can have a knock-on effect for the microbial communities that colonize our skin – reflected by the fact that as the gestational period increases, better skin bacterial richness is seen in the first four weeks of life [13].
Other physiological conditions also play a role – for instance, sebum secretion increases sharply for several days following birth before decreasing, which influences the success of certain skin microbes [9,14].
The skin microbiome evolves to an infant skin-like profile days after birth. By 4–6 weeks, infant skin microbiome structure and function have already significantly expanded and diversified, with prominent body site specificities similar to those of the maternal skin microbiome [8,15]. The microbial community then continues to evolve, mature and increase in diversity throughout a longer period of infancy and through puberty, before reaching a more stable composition that remains for adulthood [8,12] (Fig. 1).
Impact on skin health and disease
Establishing a healthy skin microbiome early on in life is essential to limit the growth of harmful or infectious microbes on our skin, and for the development of our immune system – with the effects also extending to protection later in adult life [12,15].
The presence of certain skin-resident microbes during the neonatal period can establish immune tolerance or an effective immune response to these same bacteria later in life [16]. One example of the importance of early life microbial colonization can be seen by looking at allergic and inflammatory diseases, such as atopic dermatitis.
Atopic dermatitis – the most common form of eczema – is a chronic skin condition characterized by dry skin and intense itching, with typical onset in infancy. Skin barrier dysfunction and inflammation contribute to the development of atopic dermatitis, but a link to microbiome dysbiosis (disruption) has also been demonstrated [12,17,18] – namely, a reduction in skin microbial diversity and increased presence of the bacteria Staphylococcus aureus (as well as Staphylococcus epidermidis and Malassezia bacteria) [12,17,19].
Developing a diverse skin microbiome early in life may help with this condition. It is thought that colonization with Staphylococcus bacteria during infancy may be critical for atopic dermatitis prevention as this triggers modulation of the skin’s immune system to tolerate these bacteria. Research has found that infants who had atopic dermatitis at 1 year of age had significantly less Staphylococcus bacteria around the inner elbow at age 2 months compared with unaffected infants. Yet there were no lasting differences in the skin microbiome composition between the two groups at 1 year of age, suggesting that it was early exposure to Staphylococcus that prevented atopic dermatitis [20].
Skincare and therapy opportunities
As skin microbiome development during the postnatal period and through infancy plays a critical role in skin condition and health, it follows that we should pay close attention to infant skin care – and even consider microbial therapeutic intervention – to help prevent or manage skin disease [12,15].
Day-to-day skincare
Neo- and postnatal skincare involves certain challenges, such as the loss of water two-times fast than adult skin (due to smaller cells and thinner skin) and skin pH imbalances. It is also essential to protect or enhance the developing microbiome, where it has been shown that high microbial richness and diversity is key [21].
Skincare routines should therefore support the infant’s developing skin by helping to mature and maintain the integrity of the skin barrier and microbiome, also avoiding changes in skin pH, with products such as cleansers and moisturizers that are mild and specifically formulated for the unique needs of neo- and postnatal skin [21].
Therapeutics for skin disease
Although the dynamic state of the infantile microbiome can lead to disease if disrupted, this also provides opportunities for medical intervention – an understanding that has led to an explosion of interest in the potential of microbial-based therapeutics to treat or manage skin disease [12].
In the case of atopic dermatitis, therapies typically aim to restore skin barrier health and reduce inflammation. However, current therapies, including topical corticosteroids, calcineurin inhibitors, antibiotics and bleach baths, all increase bacterial diversity during a flare-up [10]. Emollients (medical moisturizers) containing topical corticosteroids, for example, significantly reduce the abundance of Staphylococcus aureus in atopic dermatitis skin, with a consequent increase in other bacteria that are typical residents of healthy skin: Cutibacterium, Corynebacterium and Streptococcus [22]. Regular use of such emollients in infants has been shown to lead to an overall increase microbial richness, also supporting skin barrier integrity and health [15].
Explore more microbiome basics in the How it works section of the Content Hub and follow us on Instagram for the latest updates!
References
1. Capone, K. A. et al. Diversity of the human skin microbiome early in life. J. Invest. Dermatol. 131, 2026–2032 (2011).
2. Leung, M. H. Y., Wilkins, D. & Lee, P. K. H. Insights into the pan-microbiome: skin microbial communities of Chinese individuals differ from other racial groups. Sci. Rep. 5, 11845 (2015).
3. Ying, S. et al. The influence of age and gender on skin-associated microbial communities in urban and rural human populations. PLoS ONE 10, e0141842 (2015).
4. Shibagaki, N. et al. Aging-related changes in the diversity of women’s skin microbiomes associated with oral bacteria. Sci. Rep. 7, 10567 (2017).
5. Leyden, J. J. et al. Age-related changes in the resident bacterial flora of the human face. J. Invest. Dermatol. 65, 379–381 (1975).
6. Bouslimani, A. et al. Molecular cartography of the human skin surface in 3D. Proc. Natl. Acad. Sci. USA 112, 2120–2129 (2015)
7. McGinley, K. J. et al. Regional variations in density of cutaneous Propionibacteria: correlation of Propionibacterium acnes populations with sebaceous secretion. J. Clin. Microbiol. 12, 672–675 (1980).
8. Luna, P. C. et al. Skin microbiome as years go by. Am. J. Clin. Dermatol. (2020).
9. Byrd, A. L. et al. The human skin microbiome. Nat. Rev. Microbiol. 16, 143-155 (2018).
10. Schneider, A. M. & Nelson, A. M. Skin microbiota: Friend or foe in pediatric skin health and skin disease. Pediatr Dermatol. 36, 815-822 (2019).
11. https://www.biocodexmicrobiotainstitute.com/en/pro/factors-affecting-skin-microbiota
12. Shoch, J. J. et al. The infantile cutaneous microbiome: a review. Pediat. Dermatol. (2019).
13. Pammi, M. et al. Development of the cutaneous microbiome in the preterm infant: a prospective longitudinal study. PLoS ONE (2017).
14. Egert, M. et al. The Association of the skin microbiota with health, immunity, and disease. Clin Pharmacol Ther. 102, 62-69 (2017).
15. Telofski, L. et al. Effects of emollient use on the developing infant skin microbiome. Pediatrics (2020).
16. Scharschmidt, T. C. et al. A wave of regulatory T cells into neonatal skin mediates tolerance to commensal microbes. Immunity 17, 1011–1021 (2015).
17. Powers, C. E. et al. Microbiome and pediatric atopic dermatitis. J. Dermatol. 42, 1137-1142 (2015).
18. Totté, J. E. E. e tal. Prevalence and odds of Staphylococcus aureus carriage in atopic dermatitis: a systematic review and meta-analysis. Br. J. Dermatol. 175, 687-695 (2016).
19. Kong H, H. et al. Temporal shifts in the skin microbiome associated with disease flares and treatment in children with atopic dermatitis. Genome Res. 22, 850-859 (2012).
20. Kenned, E. A. et al. Skin microbiome before development of atopic dermatitis: early colonization with commensal staphylococci at 2 months is associated with a lower risk of atopic dermatitis at 1 year. J. Allergy Clin. Immunol. 139, 166-172 (2017).
22. Glatz, M. et al. Emollient use alters skin barrier and microbes in infants at risk for developing atopic dermatitis. PLoS ONE 13, e019244 (2018).
