We have known for a long-while that there is an important connection between maternal health and the health of the baby – this has evolved from, perhaps, a ‘mother’s instinct’ to scientifically-sound knowledge. Now, we have an expanding evidence base that takes this further and shows just how crucial the maternal microbiome is on the developing infant – and its microbiome.
The maternal gut microbiome is central to the health of a developing foetus, particularly its immunity which helps the infant stay protected against a range of diseases. (The vagino-uterine microbiome, and the transfer of microbiota from mother to foetus were covered previously here.)
The gut is the most heavily populated microbial site – it is no surprise that this has been a focus of many studies. It has been shown that the maternal gut microbiome has a strong influence on the infant microbiota during pregnancy. Indeed, maternal gut bacterial strains have been found to be more persistent in, and well adapted to, the infant gut compared to bacterial strains from other sources.
During pregnancy, the foetus is provided nutrients and other molecules – including from the maternal microbiome – via the placenta and umbilical cord and, after birth, via breast milk. This gestational period is a crucial time for the development of the foetus and, vitally, its immune system. As such, influences during this time are key in determining the child’s predisposition to diseases later in life. Such influences include a range of factors, primarily maternal diet, but also toxins, medication, stress, smoking and so on, which affect immunity through various mechanisms – including through altering the composition of the microbiome.
Nutrition & foetal immunity
 There’s no doubt that what a person eats during pregnancy – maternal nutrition – is vital in supporting growth of a developing foetus. Research has shown that reduced maternal malnutrition, and the resulting adaptation of a foetus, has long-lasting negative consequences on the child’s health. For example, poor foetal growth as the result of insufficient nutrition during pregnancy is associated with increased adiposity (fat) later in life when adequate nourishment is available and, in turn, an increased risk of cardiovascular disease and type 2 diabetes. Lower birth weight has also been linked to increased susceptibility to a range of health conditions in later life including osteoporosis, depression, and prostate tumors.
There’s no doubt that what a person eats during pregnancy – maternal nutrition – is vital in supporting growth of a developing foetus. Research has shown that reduced maternal malnutrition, and the resulting adaptation of a foetus, has long-lasting negative consequences on the child’s health. For example, poor foetal growth as the result of insufficient nutrition during pregnancy is associated with increased adiposity (fat) later in life when adequate nourishment is available and, in turn, an increased risk of cardiovascular disease and type 2 diabetes. Lower birth weight has also been linked to increased susceptibility to a range of health conditions in later life including osteoporosis, depression, and prostate tumors.
Ultimately, malnutrition impacts foetal immunity and its ability to fight infection, through several different means.
Lack of nutrition directly affects the development of a foetus’ white blood cells (leukocytes). It also leads to stress responses in both the mother and the growing foetus which affects the function of the placenta and foetal immune development.
Nutrition is vital to ensuring that the foetus receives antibodies from the mother, which provide so called ‘immune memory’ to pathogenic and commensal members of the microbiome. Therefore, malnutrition negatively impacts maternal antibody production weakening the defense of both mother and foetus against harmful microbes.
Indeed, the foetus’ developing immune system is largely shaped by the uterine environment and reduced immunity in utero has long-term effects. We see this effect both in children and adults, including increased vulnerability to immune-related diseases such as allergic and autoimmune diseases: asthma, type 1 diabetes and inflammatory bowel disease (IBD), as well as skin disorders.
The impact of the maternal gut microbiome on nutrition
So, it’s clear that good maternal nutrition is vital for the healthy development of an infant’s immune system. But, how does the microbiome contribute to the general nutritional state during pregnancy?
Well, the microbiome has several well-known benefits:
- Increase the efficiency of energy extraction from food. Digestion involves the breakdown of large insoluble food molecules into small water-soluble food molecules so that they can be absorbed into the blood plasma. Beyond the body’s own mechanical and chemical processes of digestion, the mother’s gut microbiome further contributes to the metabolism of dietary components in the intestine by digesting complex carbohydrates – such as peas, beans, whole grains, and vegetables – which are resistant to our own digestive enzymes. As such, the microbiome contributes to the absorption of micronutrients into the mother’s, and subsequently the foetus’, body.
- Provide vitamins. Gut microbes are required for the synthesis of vitamins – organic compounds essential for normal growth and nutrition. Of course, the action of gut microbes cannot substitute for a healthy, balanced diet which provides us with essential vitamins and from which gut microbes salvage energy. The metabolic capability of microbes enables the production of vitamins and this is particularly true for vitamin K. Fascinatingly, evidence has shown that animals raised in germ-free conditions did not generate vitamin K and, as a result, had a tendency to bleed easily (bleeding diathesis) due to impaired clotting factor synthesis usually supported by vitamin K. B vitamins – including folate (vitamin B9) and vitamin B12 – also rely on synthesis by the microbiome rather than the body’s own processes. This takes place primarily in the large intestine where uptake into the blood is more restricted than in the small intestine. However, while most newly synthesized vitamins are excreted by the body, there is evidence that B vitamins are sourced from microbes. Folate is needed for healthy growth and development as so is important for pregnancy since it can help prevent birth defects including neural tube defects, such as spina bifida, facial clefting, and cardiac defects. In developed countries, pregnant woman are widely supplemented with folate to prevent such conditions occurring.
- Metabolise xenobiotics – foreign chemical substances, such as those from plant or pharmaceutical sources. Uptake of xenobiotics, whether drugs, pollutants, pesticides, food additives, etc., can affect the maternal microbiome and, secondarily, the microbiome of offspring. Studies have provided evidence of antibiotics affecting the gut microbiome e.g. increased Enterobacteriaceae bacteria has been observed with the intake of the antibiotic vancomycin due to reduced competition. The selectivity of antibiotics’ effects on the gut microbiome has proven beneficial in treating gut microbiome-related diseases. Public health studies have shown that air pollution exposure is associated with a range of health effects – including gastrointestinal diseases, the development of which involves the gut microbiome. Within the pregnancy context, a drug that was once prescribed to pregnant women to prevent miscarriage was later identified as the cause for infertility and tumors in adult life. This is an extreme example and xenobiotics are largely no cause for concern as the gut microbiome has a powerful ability to metabolise xenobiotic chemicals. Indeed, the maternal gut assists with the metabolism of many environmental and pharmaceutical xenobiotics thereby reducing exposure of the foetus to these chemicals.
The impact of nutrition on the maternal and foetal microbiome
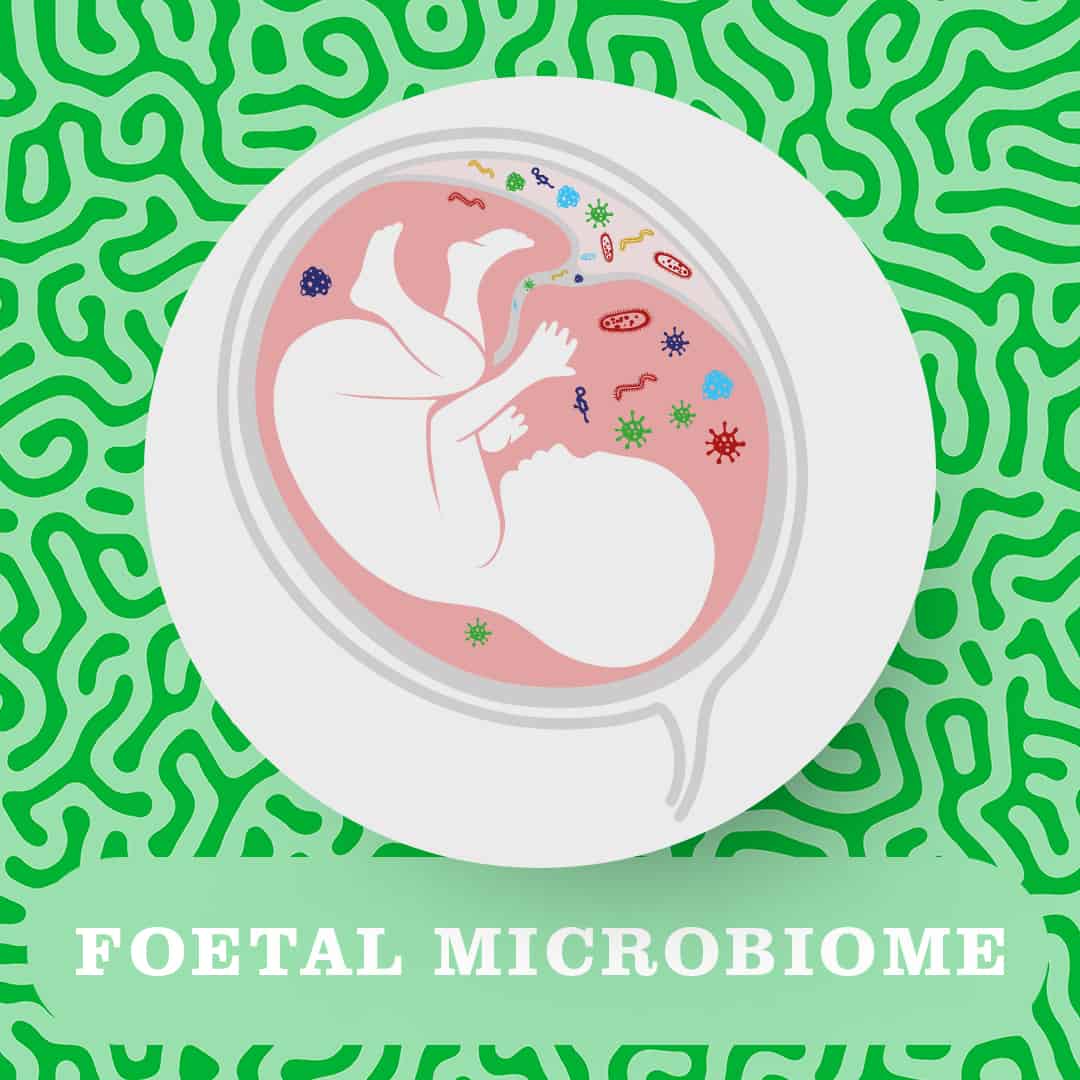
While the microbiome affects the food we ingest, maternal diet itself also shapes the composition of the maternal gut microbiome. It is likely that the quantity of microbes in the small intestine increases during pregnancy and, as such, the exchange of micronutrients between the microbiome and the body likely also increases with subsequent effects on the foetus.
Indeed, the impact of nutrition on the gut microbiome, in turn, affects the development of the foetal immune system via metabolites secreted by healthy bacteria. For example, soluble dietary fibres are fermented by gut bacteria into short chain fatty acids (SCFAs) which have been shown to improve the immune system of offspring. The long-term prevention of allergies and metabolic diseases in the foetus and newborn may therefore be supported by consumption of a soluble high fiber diet during pregnancy and lactation. Such foods could include vegetables, such as mushrooms, and even seaweed!
Summary
It’s clear that a complex, bi-directional relationship exists between a mother and child during and soon after pregnancy with nutrients and microbes being exchanged via the placenta, umbilical cord and breast milk.
This exchange enables the maternal gut microbiome to contribute to the development of the foetus – especially its immune system which protects against infection from harmful microbes (including those on the skin!). Of course, nutrition is vital for growth and development and helps ‘feed’ the maternal and foetal gut microbiome but the gut microbiome has also been shown to play several roles in how we as humans receive nutrients and vitamins and the implications of this during pregnancy.
Want to know more? Catch up with the Maternal Microbiome:
Part 1 or browse more Microbiome Basics content in the How it
works section of the Content Hub.
Remember to follow us on Instagram to receive the latest updates!
References:
Lu et al, 2015 – ILAR Journal
Macpherson et al, 2017 – Nature Reviews Immunology
Nyangahu & Jaspan, 2019 – The Journal of Translational Immunology
Nakajima et al, 2020 – Bioscience of Microbiota, Food and Health
